Researchers at Vanderbilt Health have uncovered significant findings regarding the effects of weight loss drugs and bariatric surgery on body composition in patients with obesity. The study reveals that both interventions lead to a moderate loss of fat-free mass, including lean muscle, alongside a substantial reduction in fat. This discovery is crucial as a higher percentage of fat mass is linked to increased mortality risk from obesity-related diseases, while a higher percentage of fat-free mass offers protective benefits.
The research, published on January 9 in the journal JAMA Network Open, emphasizes the need for further studies to understand how fat mass (FM) and fat-free mass (FFM) change post-bariatric surgery or treatment with GLP-1 receptor agonist drugs in real-world clinical settings. The study was spearheaded by Danxia Yu, PhD, an associate professor of Medicine in the Division of Epidemiology, and Jason Samuels, MD, an assistant professor of Surgery.
Study Methodology and Key Findings
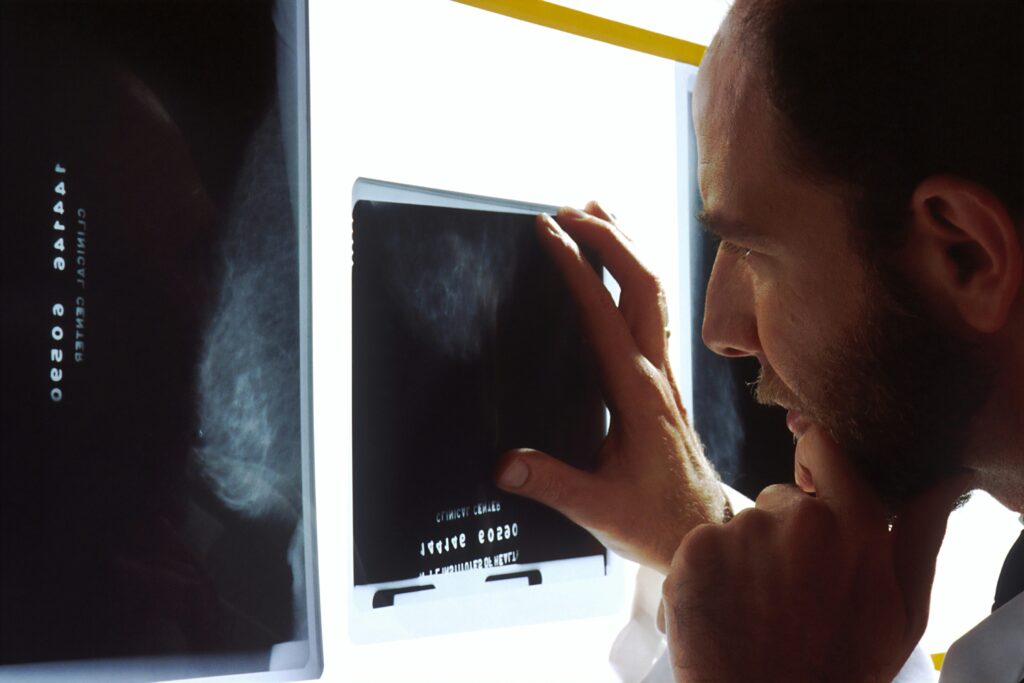
This retrospective study analyzed electronic health records from 1,257 patients aged 18 to 65 who underwent bariatric surgery at Vanderbilt Health between 2017 and 2022, and 1,809 patients treated with the drugs semaglutide or tirzepatide from 2018 to 2023. Exclusions were made for individuals with a history of end-stage renal disease or congestive heart failure.
Body composition was assessed using bioelectrical impedance analysis, which estimates FM and FFM based on various individual characteristics such as height, weight, age, race, gender, history of diabetes, and duration of GLP-1 treatment. The findings indicated that over a 24-month period, both medical and surgical weight loss approaches resulted in significant reductions in FM, modest reductions in FFM, and increased FFM/FM ratios, signifying improved body composition. Notably, male patients demonstrated better long-term preservation of FFM compared to female patients.
“Over 24 months, both medical and surgical weight loss approaches led to significant reductions in FM, modest reductions in FFM, and increases in the FFM/FM ratio, reflecting improved body composition.”
Implications and Future Research
The results of this study underscore the potential of weight loss interventions in enhancing body composition, which could subsequently reduce the risk of obesity-related health issues. However, the researchers call for more comprehensive studies to explore these effects in diverse clinical settings. The variability in outcomes between male and female patients also highlights the need for personalized approaches in obesity treatment.
According to expert opinions, understanding the balance between fat and lean mass is vital for developing effective weight management strategies. The study’s findings could pave the way for more targeted therapies that optimize body composition, thereby improving overall health outcomes for individuals struggling with obesity.
Expert Contributions and Support
The research team included first authors Zicheng Wang, MS, a graduate student, and Lei Wang, PhD, a postdoctoral fellow in Epidemiology. Other contributors were Xinmeng Zhang and You Chen, PhD, from Biomedical Informatics and Computer Science; Brandon Lowery from the Vanderbilt Institute for Clinical and Translational Research; Lauren Lee Shaffer, MS, and Quinn Wells, MD, from Cardiovascular Medicine; and Charles Flynn, PhD, Brandon Williams, MD, Matthew Spann, MD, and Gitanjali Srivastava, MD, from Surgery.
This study was partially funded by National Institutes of Health grants R01DK126721 and R01CA275864, highlighting the importance of continued support for research that addresses critical health challenges posed by obesity.
“The study was supported in part by National Institutes of Health grants R01DK126721 and R01CA275864.”
As the medical community continues to grapple with the complexities of obesity, this study represents a significant step forward in understanding how modern interventions can be optimized to improve patient outcomes. The ongoing exploration of these treatments will be vital in shaping future healthcare strategies aimed at combating obesity and its associated risks.