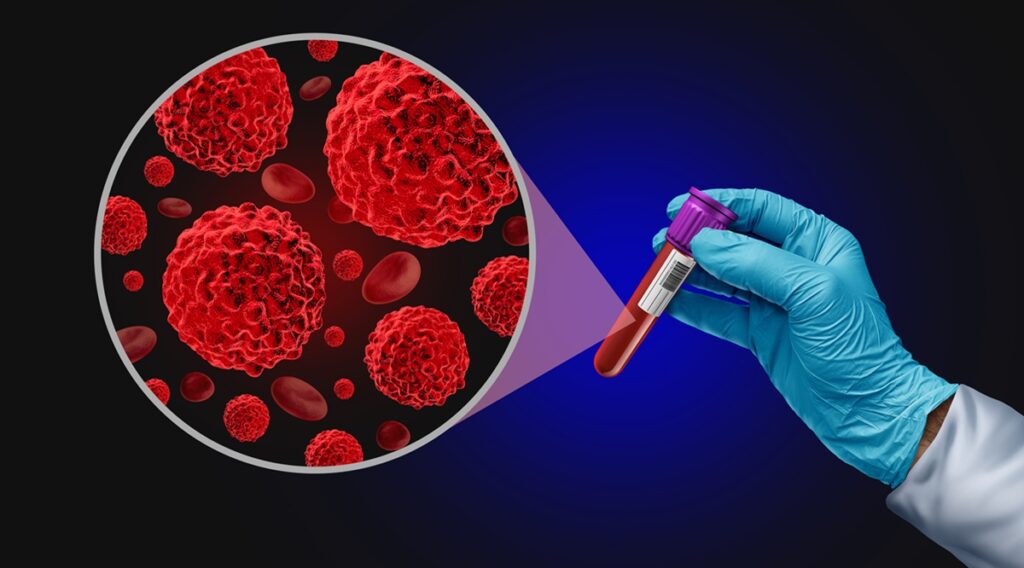
Blood Cancer screening Test as an Oncology medical diagnosis for tumor markers as a liquid biopsy for early detection with malignant cells to diagnose ovarian colon and prostate cancers.
One of the most challenging diagnoses a doctor can deliver is pancreatic cancer. According to the National Cancer Institute, only 13% of patients survive five years post-diagnosis. Despite accounting for just 3.3% of new cancer cases annually in the United States, pancreatic cancer is responsible for 8.4% of cancer deaths, making it the third deadliest cancer.
The primary reasons are late detection, rapid progression, and poor response to treatments. Currently, there are no federally approved screening tests for early detection. However, researchers at Oregon Health & Science University (OHSU) are pioneering a diagnostic tool that could change this: a liquid biopsy. This blood test aims to identify pancreatic cancer before symptoms appear, potentially allowing for earlier treatment and better outcomes.
Breakthrough in Detection
In a study involving 350 patients, both with and without pancreatic cancer, the test analyzed changes in protein activities indicative of pancreatic ductal adenocarcinoma (PDAC), the most common and lethal form of the disease. The test accurately identified healthy individuals 98% of the time and detected 73% of pancreatic cancer cases, as reported in Science Translational Medicine.
This innovation is part of a broader wave of liquid biopsies being tested for various cancers, often using blood, urine, saliva, and other bodily fluids. “Liquid biopsies show promise for discovering many cancers earlier than they are found now,” says Jasmine Zhou, PhD, professor of pathology and laboratory medicine at UCLA.
Challenges and Considerations
Despite their potential, liquid biopsies face scrutiny regarding their effectiveness and implications for treatment. The U.S. Food and Drug Administration (FDA) has approved only a few such tests, and insurance coverage is rare. Nonetheless, these tests address a significant gap, as FDA-approved screenings exist for only five cancers: breast, cervical, colorectal, prostate, and lung.
Richard M. Hoffman, MD, MPH, emeritus professor at the University of Iowa, notes that remaining cancers account for nearly half of all diagnoses and about 60% of cancer deaths. Liquid biopsies could signal cancers currently lacking screening methods, offering new hope.
Expert Insights
Hoffman, who developed guidance for primary care physicians on multi-cancer early detection (MCED) tests, emphasizes their potential. “Multi-cancer blood tests could be a game changer,” says Jagpreet Chhatwal, PhD, director at Massachusetts General Hospital and Harvard Medical School. These tests could increase early-stage diagnoses and significantly reduce late-stage cases.
How Liquid Biopsies Work
Unlike traditional biopsies that sample tissue, liquid biopsies detect cancer signals in bodily fluids. Tumors shed DNA mutations or trigger protein activities, which can be identified in these fluids. “Part of the tumor dies, and the DNA of those cells is released into the blood,” explains Jose Montoya Mira, PhD, lead researcher at OHSU.
Currently, only a few FDA-approved liquid biopsies are in routine use, such as PSA tests for prostate cancer and Cologuard for colorectal cancer. The new OHSU test, using fluorescent peptides, aims to expand detection to pancreatic cancer, showing 93% accuracy overall.
Future Directions
The initial study was retrospective, but OHSU researchers are now analyzing a prospective cohort to validate the test’s performance in real-time. They are also seeking partners for clinical trials, focusing on high-risk patients who would benefit most from early detection.
Balancing Benefits and Risks
While promising, liquid biopsies raise questions about accuracy, cost, and implications of results. Most are still in development, and the FDA has not approved MCEDs due to a lack of conclusive trial results. “We’re looking for results showing that screening for multiple cancers will reduce overall cancer mortality,” Hoffman states.
Positive results from liquid biopsies often lead to surgical biopsies for confirmation, which can be costly and distressing. “You’re telling somebody, ‘You have cancer.’ That’s super-stressful,” Montoya Mira notes.
Cost and Accessibility
With few FDA approvals, most liquid biopsies are not covered by insurance, leaving patients to bear the cost. “If you get a positive result, who’s paying for the follow-up?” Montoya Mira asks, highlighting the financial burden.
Moreover, these tests should supplement, not replace, existing screenings. “People might think they can skip other tests because they got this [liquid test] and it was negative,” Chhatwal cautions.
The Path Ahead
While universal testing for all cancers is not yet feasible, focusing on high-risk populations is a reasonable approach. Zhou suggests targeting those with a family history, exposure to carcinogens, or older age. Hoffman agrees, emphasizing the need for clinician guidance to manage patient expectations.
“The challenge for clinicians is that patients will see MCED testing as an exciting new screening technology,” Hoffman says. “Clinicians have to temper that enthusiasm and educate patients about the current limitations.”
Despite these challenges, the potential of liquid biopsies for early cancer detection is significant. Continued research and development are crucial as this technology evolves, representing a major step forward in the fight against cancer.