An abbreviated version of the Brain Care Score (BCS) has shown promise in predicting the risk of dementia, stroke, and late-life depression, according to a recent study published in Neurology Open Access. The study highlights the potential of this simplified tool to offer insights into brain health, particularly in settings where access to comprehensive medical assessments may be limited.
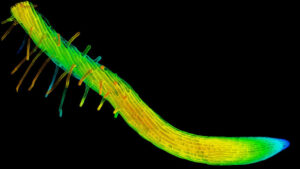
The Brain Care Score is a validated 21-point scale designed to evaluate the risk of neurological and psychological conditions based on modifiable factors such as physical health, lifestyle, and social-emotional well-being. However, the full BCS requires physical measures that involve blood collection, which can be a barrier in certain clinical or community environments. The abbreviated version, by contrast, focuses on seven lifestyle and social-emotional components, making it more accessible.
Study Insights and Findings
Researchers from the University of Alabama at Birmingham and Massachusetts General Hospital conducted an extensive analysis using data from the UK Biobank. The study involved 397,515 adults aged 40 to 69 years, who were assessed with both the full and abbreviated BCS. The study aimed to evaluate the correlation between BCS scores and the incidence of dementia, stroke, and late-life depression over a follow-up period.
At a median follow-up of 13.2 years, 2.1% of participants had a stroke, 1.6% developed dementia, and 3.1% experienced late-life depression.
The findings revealed a strong correlation between the abbreviated and full BCS, with Pearson and Spearman correlation coefficients of 0.70 and 0.66, respectively (both P <.001). Moreover, individuals with medium and high BCS scores were found to have a lower risk for these conditions compared to those categorized as low risk.
Implications for Remote Health Assessment
The study underscores the potential of the abbreviated BCS in remote health assessments, particularly for communities with limited access to traditional healthcare services. The ability to predict neurological and psychological risks using a simplified tool could revolutionize how brain health is monitored in underserved areas.
“Our findings show that remote assessment of brain care has the potential to serve communities lacking traditional health care access,” the study authors noted.
However, the study also highlighted limitations, such as the lack of racial and ethnic diversity in the cohort, which could affect the generalizability of the results.
Comparative Analysis and Expert Opinions
In comparison to the full BCS, the abbreviated version demonstrated slightly less precision in predicting risks. For instance, medium BCS scores were associated with adjusted hazard ratios (aHRs) of 0.68 for stroke using the full BCS and 0.75 with the abbreviated version. Similarly, high scores showed aHRs of 0.55 and 0.76, respectively.
For dementia, medium BCS scores were associated with aHRs of 0.86 (full) and 0.80 (abbreviated), while high scores correlated with aHRs of 0.87 and 0.92.
Experts suggest that while the abbreviated BCS may not replace the full version, it offers a valuable alternative for initial screenings and ongoing monitoring, especially in resource-limited settings.
Future Directions and Considerations
Looking ahead, researchers emphasize the need for further studies to explore the applicability of the abbreviated BCS across diverse populations. Enhancing the tool’s accuracy and expanding its use could significantly impact public health strategies aimed at preventing dementia, stroke, and depression.
As the healthcare landscape continues to evolve, tools like the abbreviated BCS could play a crucial role in bridging gaps in care and ensuring that more individuals have access to essential health assessments.
For more detailed disclosures and affiliations of the study authors, readers are encouraged to refer to the original publication in Neurology Open Access.