It was a typical Monday morning for Rishi Tandon, a 29-year-old graphic designer in Bengaluru. Determined to tackle his task list, he sat at his desk with emails to address, client work to complete, and a presentation due by the afternoon. Yet, as the hours slipped by, Rishi found himself aimlessly switching between browser tabs, watching unrelated videos, and staring blankly at his screen. His mind refused to settle.
When his manager called to inquire about the presentation, Rishi panicked—he hadn’t even started. He apologized, attributing his lapse to a poor night’s sleep, but deep down, he recognized this pattern. Friends often labeled him as “scattered” or “easily distracted,” comments he would laugh off. However, recently, it felt like he was losing control of his own mind.
Unbeknownst to Rishi, he was not alone. He was living with undiagnosed adult attention-deficit/hyperactivity disorder (ADHD), a condition often misperceived as a childhood disorder predominantly affecting hyperactive young boys in classrooms. The reality, however, is far more complex.
ADHD: A Global Perspective
ADHD is a common neurodevelopmental disorder that affects children and often persists into adulthood. According to a World Health Organization report, approximately 5 percent of children globally are diagnosed with ADHD. A systematic review of global ADHD prevalence from 2020 onward reveals significant variations, largely influenced by differences in diagnostic methods and study quality.
Survey-based studies, particularly in Asia, often report inflated prevalence rates due to reliance on self-reports and less rigorous methodologies. Conversely, studies utilizing medical records or clinical interviews, more prevalent in North America and parts of Europe, present more conservative estimates. For instance, ADHD prevalence in children ranges from 3.2 percent in Sweden to 10.5 percent in the United States.
Evidence suggests higher rates among older children compared to younger ones, with slight increases in recent years.
The COVID-19 pandemic temporarily disrupted ADHD diagnosis and treatment, causing a dip in prescription rates in 2020, followed by a rise in 2021. This reflects healthcare access issues rather than actual changes in prevalence.
Diagnosis Challenges and Regional Variations
Despite increasing demand and reports of long waiting lists for ADHD assessments, reliable data on referrals and diagnosis conversion rates remain scarce. A 2024 research study in India indicated prevalence rates ranging from 1.3 percent to 28.9 percent, with higher rates among males. However, many cases, particularly among females and minority groups, go undiagnosed due to cultural and systemic barriers.
Diagnosis and treatment of ADHD vary widely across regions, largely due to gaps in healthcare, research, and professional training. Although national mental health policies exist, their implementation is inconsistent. Improving diagnosis and support in India requires more trained professionals, better school support, and culturally sensitive interventions.
A systematic review found that adult ADHD is quite common in India, with prevalence rates ranging from 5.48 percent to 25.7 percent across various population groups.
The Adult ADHD Experience
Adult ADHD often presents differently from its childhood counterpart. Individuals like Rishi may not exhibit classic hyperactivity. Instead, they may silently battle chronic inattention, forgetfulness, impulsivity, and emotional dysregulation. It’s not about a lack of willpower or motivation—it’s a neurological condition.
Adults with ADHD are significantly more likely to experience job instability, relationship difficulties, and mood disorders compared to their non-ADHD peers. They also report more frequent legal troubles and financial struggles. ADHD affects multiple areas of life: projects remain unfinished, daily routines disintegrate, appointments are forgotten, and conversations become challenging to follow.
This can lead to a cycle of low self-esteem and chronic anxiety.
Understanding and Managing ADHD
The emotional toll of untreated ADHD can be devastating. Adults often feel as though they are constantly underperforming, regardless of their efforts. Many describe a sense of internal chaos or frustration at their inability to control their thoughts. Over time, this may lead to comorbid conditions such as depression, anxiety, and even substance abuse.
It’s not just the individual who suffers. Partners, friends, and family members are often affected too. Without understanding the underlying issues, ADHD behaviors are frequently misinterpreted as laziness, irresponsibility, or lack of care, which can strain relationships and lead to caregiver burnout.
With a 70-80 percent heritability rate, ADHD is among the most strongly inherited psychiatric conditions.
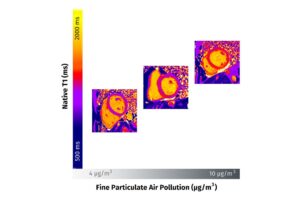
Genetic factors play a significant role, with genes involved in dopamine transmission commonly associated with the disorder. People with ADHD often have smaller brains and delayed brain maturation, particularly in areas like the amygdala, hippocampus, and frontal cortex, which are involved in emotion regulation, memory, and cognitive functions.
Moving Forward: A Roadmap for Change
For someone like Rishi, understanding his condition can be transformative. A diagnosis isn’t a label—it’s a roadmap. It offers validation and opens doors to effective treatments, which may include cognitive behavioral therapy (CBT), medication, and environmental or behavioral modifications. CBT, in particular, helps individuals identify and challenge negative thought patterns and behaviors, improving emotional regulation and developing coping strategies.
Once equipped with the right tools, many adults with ADHD discover untapped potential. They often possess high levels of creativity, intuition, and energy, especially in environments that allow flexibility and autonomy.
What’s most important is to shift how ADHD is viewed. It’s not about being lazy or undisciplined—it’s about having a brain that works differently and needs different kinds of support. For both children and adults, compassion, awareness, and proper intervention are far more effective than judgment or criticism.
Asking for help is not a weakness; it’s the beginning of clarity.
Understanding ADHD is not just about naming a disorder—it’s about finding hope, building strategies, and realizing that success and wellness are still within reach.