When Karina Ledesma’s kidneys failed during her high school years, she faced the daunting prospect of a transplant followed by a lifetime on immunosuppressive drugs. However, thanks to an experimental clinical trial at UCLA, she now lives with a kidney donated by her sister and no longer requires daily medication to protect it.
“It was such a relief to finally throw all the drugs away,” said Ledesma, 26. “I didn’t need to keep them here. I didn’t need to see them every day as a reminder. Tossing them all out was just a really great feeling.”
For nearly a year post-transplant, and before joining the trial, Ledesma suffered from the side effects of immunosuppressive medications, including insomnia, burning sensations in her extremities, and the constant need to schedule her day around medication times. Now, she is free from these burdens, supported by her sister Rosa Rivera, 28, who donated the kidney.
UCLA’s Groundbreaking Clinical Trial
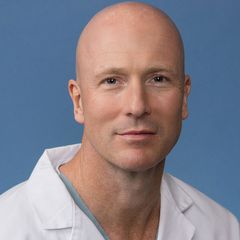
More patients may soon share Ledesma’s experience. Dr. Jeffrey Veale of UCLA has secured a $6.7 million grant from the California Institute for Regenerative Medicine to expand the clinical trial that aided Ledesma. His study investigates delayed immune tolerance, which involves infusing donor-derived blood stem cells months or years after a kidney transplant to retrain the recipient’s immune system, potentially eliminating the need for lifelong immunosuppressive drugs.
Veale and his team have already achieved early success with this approach, initially focusing on patients with a close-sibling match who had their transplant within the last five years. Starting in January 2026, the trial will open to patients with transplants up to 20 years old.
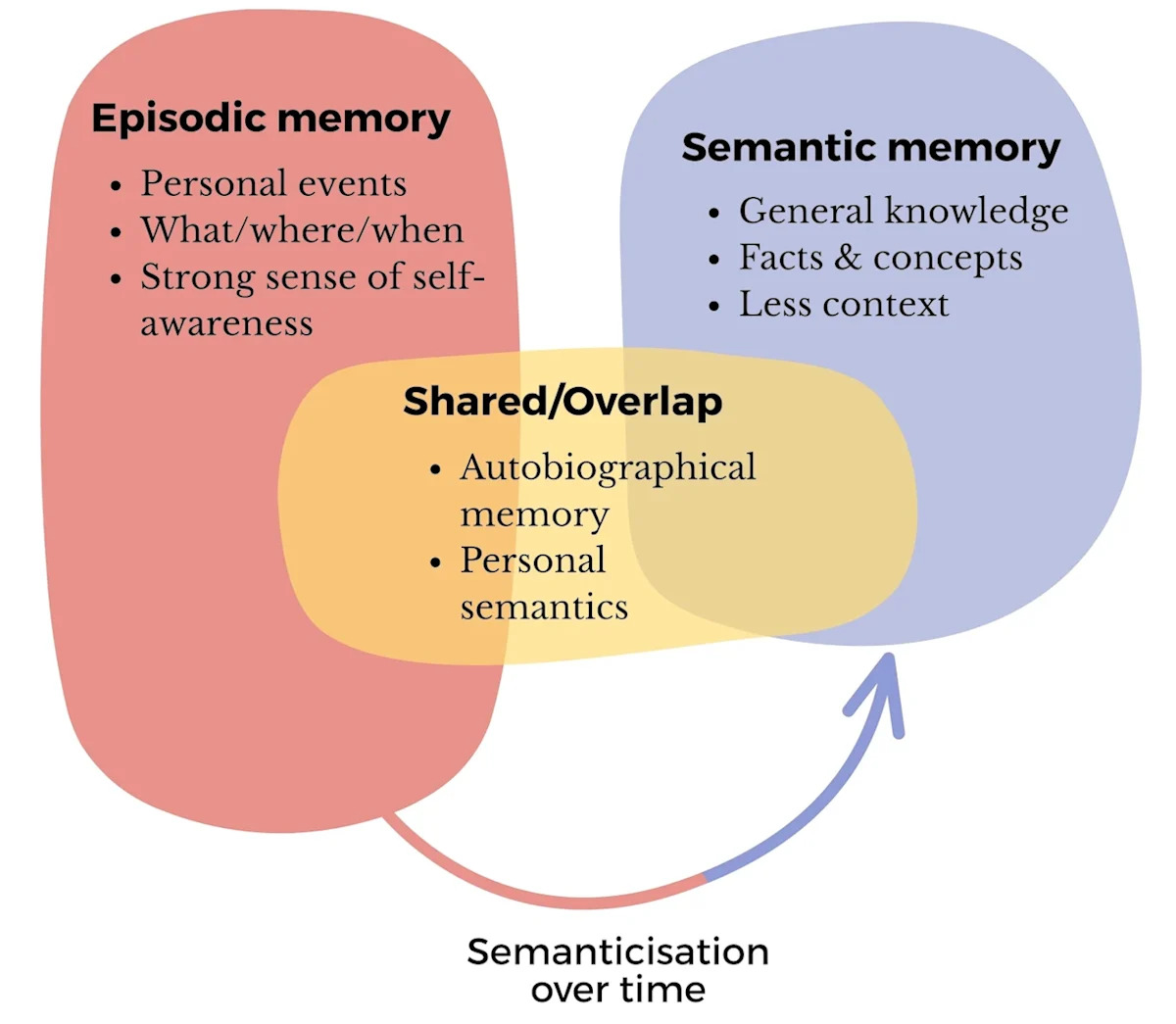
The Science Behind Delayed Immune Tolerance
The method works by integrating donor stem cells into the recipient’s bone marrow and immune system, creating a mixed population of donor and recipient immune cells, known as chimerism. This helps the recipient’s immune system recognize the transplanted kidney as “self,” reducing rejection risk and eliminating the need for ongoing immunosuppressive medications.
“This could be the difference between managing end-stage renal disease as a chronic condition and actually curing it,” said Veale, professor of urology at the David Geffen School of Medicine at UCLA.
Of the six patients treated in the phase 1/2 trial, three are completely off immunosuppressive drugs, while others are on reduced doses or successfully tapering.
Expanding the Trial and Its Implications
The new grant will enable the enrollment of 10 additional patients and support research into the science of immune tolerance. This will help Veale and his team identify biological mechanisms that make tolerance possible and uncover biomarkers predicting which patients will benefit most.
Currently, the trial is limited to patients who have received a kidney donation from a well-matched sibling. Veale aims to extend this to a broader range of donor-recipient types and other organ transplant cases.
“If we can understand why tolerance works at the cellular level, we may be able to offer it to patients with less well-matched donors — or even extend it to liver and other transplants,” Veale explained.
Challenges and Opportunities
Immunosuppressive medications, while vital for transplant success, pose serious side effects, including infections, cardiovascular disease, diabetes, and cancer. Ironically, they can also damage the organ they are meant to protect.
“These immunosuppressive drugs have not changed in decades,” Veale noted. “They’re expensive, impair the recipient’s quality of life, and decrease graft survival.”
Approximately half of all kidney transplants fail within 15 years, with many of the 90,000 people currently awaiting a kidney in the U.S. needing subsequent transplants. Delayed tolerance could change this trajectory.
Understanding the Mechanisms of Tolerance
Veale’s team will use the CIRM funding to analyze blood and tissue samples from trial participants to uncover clues about immune cell changes, cytokine profiles, or signs of donor cells persisting in the organ. These insights could help predict patient responses and guide future trials involving mismatched pairs.
“With this funding, we can find out why tolerance works. We really don’t fully understand the immunology behind it,” Veale said.
Ultimately, Veale hopes the research will shift the transplant field’s focus from preserving organ function to preventing long-term harm, not just keeping donated kidneys working but keeping recipients healthy and medication-free.