Deep brain stimulation (DBS), a technique involving implants in the brain that function like a “pacemaker,” has shown promising results in an open-label trial, leading to clinical improvements in half of the participants suffering from treatment-resistant severe depression. This study, conducted by researchers from the UK and China, not only demonstrated the efficacy of DBS but also identified a specific brain activity signature that could predict patient response to the treatment, potentially paving the way for more targeted interventions in the future.
Major depressive disorder, a prevalent and debilitating mental health issue worldwide, often resists conventional treatments such as antidepressants and cognitive therapies. Statistics reveal that treatment fails for 30% to 50% of patients with depression. Over recent decades, DBS has emerged as a viable treatment for various conditions, particularly Parkinson’s disease, by inserting electrodes deep into the brain to deliver mild electrical stimulation that corrects abnormal brain activity.
Study Details and Findings
The study, published in Nature Communications, involved 26 patients from Ruijin Hospital, Shanghai Jiaotong University School of Medicine, all diagnosed with treatment-resistant depression. The trial’s open-label nature meant that both the researchers and participants were aware of the DBS administration. The researchers targeted two specific brain regions: the bed nucleus of the stria terminalis (BNST) and the nucleus accumbens. The BNST plays a crucial role in regulating stress and anxiety, while the nucleus accumbens is pivotal in processing rewards and motivation.
Remarkably, half of the participants experienced significant improvements, as measured by various depression and anxiety symptom scores, along with quality of life and disability assessments. Notably, nine patients, accounting for 35% of the cohort, achieved remission, indicating a near-complete elimination of symptoms.
Brain Activity Patterns and Response
Researchers recorded brain electrical activity using DBS electrodes in the BNST and scalp electroencephalogram (EEG), identifying theta activity (4–8 Hz) as a critical frequency range. This theta activity correlated with the severity of depression and anxiety symptoms. Patients with lower pre-surgery theta activity levels reported more significant improvements in depression and anxiety, though not in anhedonia, the loss of pleasure.
Furthermore, patients exhibiting greater coherence between the BNST and the prefrontal cortex at theta frequencies tended to have better outcomes. This coherence suggests enhanced communication between these regions, crucial for emotional regulation.
Expert Insights and Future Directions
Professor Valerie Voon from the University of Cambridge and Fudan University, China, remarked, “Deep brain stimulation shows real promise at tackling treatment-resistant depression, which can have a huge impact on people’s lives. But our study hasn’t just highlighted this promise, it’s given us a potential and much-needed objective marker to say which patients will respond best.”
Dr. Linbin Wang, also from the University of Cambridge, added, “We found that brain activity at a particular frequency—theta brainwaves—could tell us which patients would have the best response to DBS treatment in the BNST brain region. This could help us personalize treatment for individual patients in the future.”
During the trial, DBS reduced BNST theta activity, and this reduction matched improvements in symptoms of depression and anxiety.
This discovery opens the possibility of developing a ‘closed-loop system’ that uses real-time feedback to adjust electrical stimulation. Professor Voon explained, “Because theta activity tracks anxiety states in real time, it means that if activity is high, we can say, ‘OK, this person is in an anxious state, we need to turn up stimulation.’ Likewise, if theta activity is low, we can turn down the stimulation.”
Implications and Next Steps
Professor Bomin Sun, the neurosurgeon leading the study at Shanghai Jiao Tong University School of Medicine, stated, “This is the largest study to show that deep brain stimulation of the BNST and nucleus accumbens can treat depression. Depression is a major public health problem in China and globally. This study not only tells us how the brain is impaired in depression, it also highlights the potential of DBS for depression.”
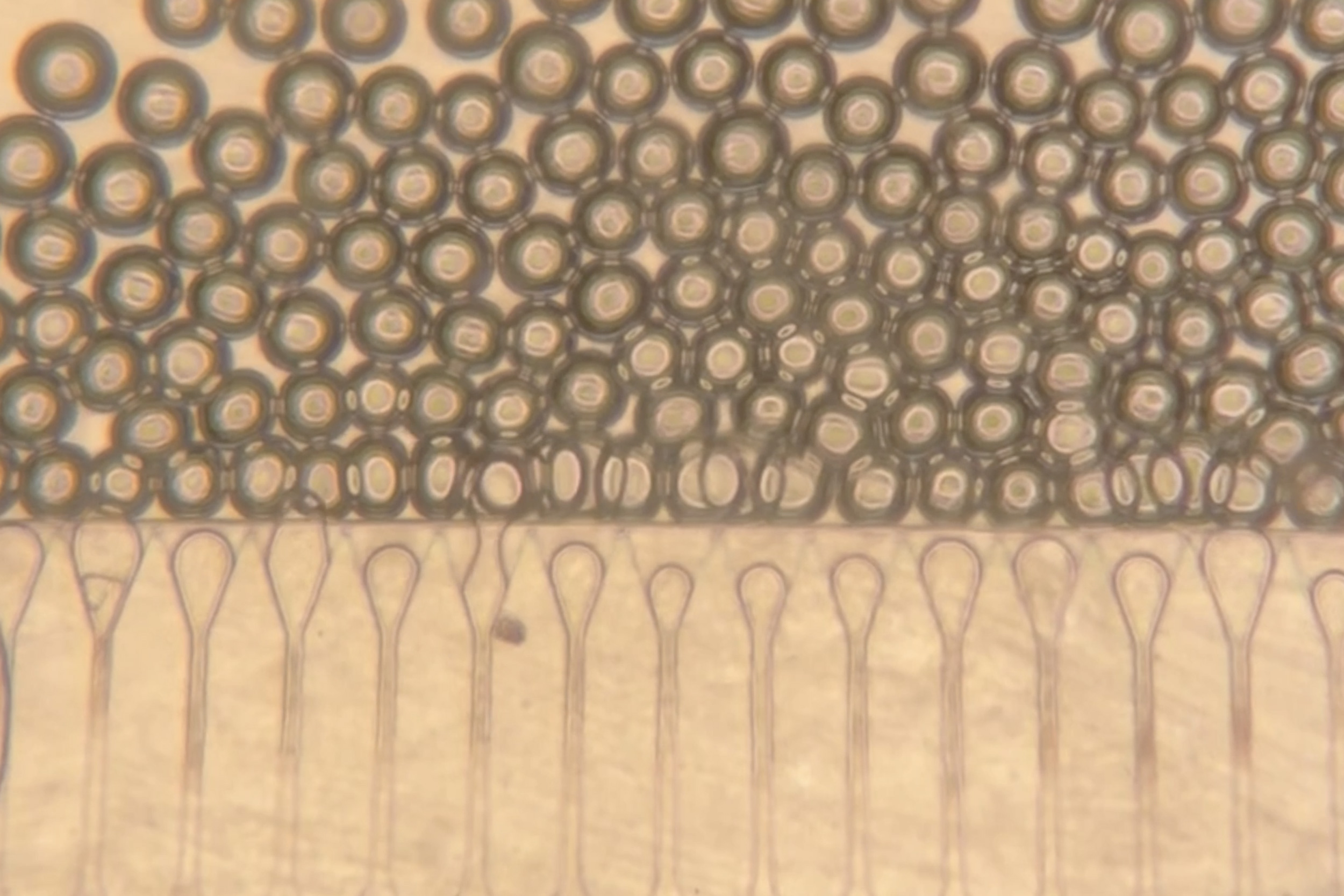
Additionally, the researchers discovered psychological measures indicating patient response to treatment. Participants exposed to various images—pleasant, neutral, and negative—showed that those with the strongest reactions to negative images were least likely to benefit from DBS.
Looking forward, these findings suggest that DBS could become a more personalized treatment option for those with severe depression and anxiety, with the potential to significantly improve quality of life for many patients worldwide. Further research will likely focus on refining the closed-loop system and exploring additional biomarkers to enhance treatment precision and efficacy.