Pinned between the stomach and spine, the pancreas plays a crucial role in digestion and blood sugar regulation. However, it is also the site of one of the most aggressive forms of cancer: pancreatic ductal adenocarcinoma (PDAC). PDAC is the most common type of pancreatic cancer and the third-leading cause of cancer-related deaths in the United States. Its stealthy nature makes it difficult to detect early, and it recurs in approximately 70% of cases after treatment. Alarmingly, only 13% of those diagnosed survive beyond five years.
In a groundbreaking study, a multidisciplinary team at the University of Illinois Chicago is investigating how lidocaine, a common local anesthetic, influences pancreatic cancer cells that are released into the bloodstream during surgery. This research, recently published in the journal Lab on a Chip, evaluates a novel method to capture these rogue cells, potentially mitigating metastasis.
Exploring the Potential of Lidocaine
Dr. Gina Votta-Velis, a professor of anesthesiology at UIC’s College of Medicine and a lead investigator, expressed optimism about the study’s implications. “I really expect that the results of this study may help our patients,” she stated. “The notion that lidocaine, which has been used to relieve pain for more than 65 years, may mitigate metastasis and favorably affect patient outcomes is highly innovative.”
In 2018, Votta-Velis received a grant from the American Society of Regional Anesthesia and Pain Medicine to explore this concept. The study focuses on circulating tumor cells (CTCs), cancerous cells that detach from the primary tumor—often during surgical removal—and enter the bloodstream. Patients with a higher presence of these aggressive CTCs tend to have poorer prognoses and higher recurrence rates.
“CTCs are the seeds of metastasis,” Votta-Velis explained. “If we can detect them and decrease their aggressiveness with lidocaine infusion, we may lower the risk of the metastatic process.”
The Role of Microfluidics in Cancer Detection
Isolating CTCs poses a significant challenge, akin to finding a needle in a haystack, as it involves extracting 30 to 40 cells from billions circulating in the bloodstream. To tackle this, Votta-Velis collaborated with Ian Papautsky, a UIC professor of biomedical engineering specializing in microfluidics. Papautsky’s expertise lies in understanding how small amounts of fluids, such as blood, flow through tiny channels.
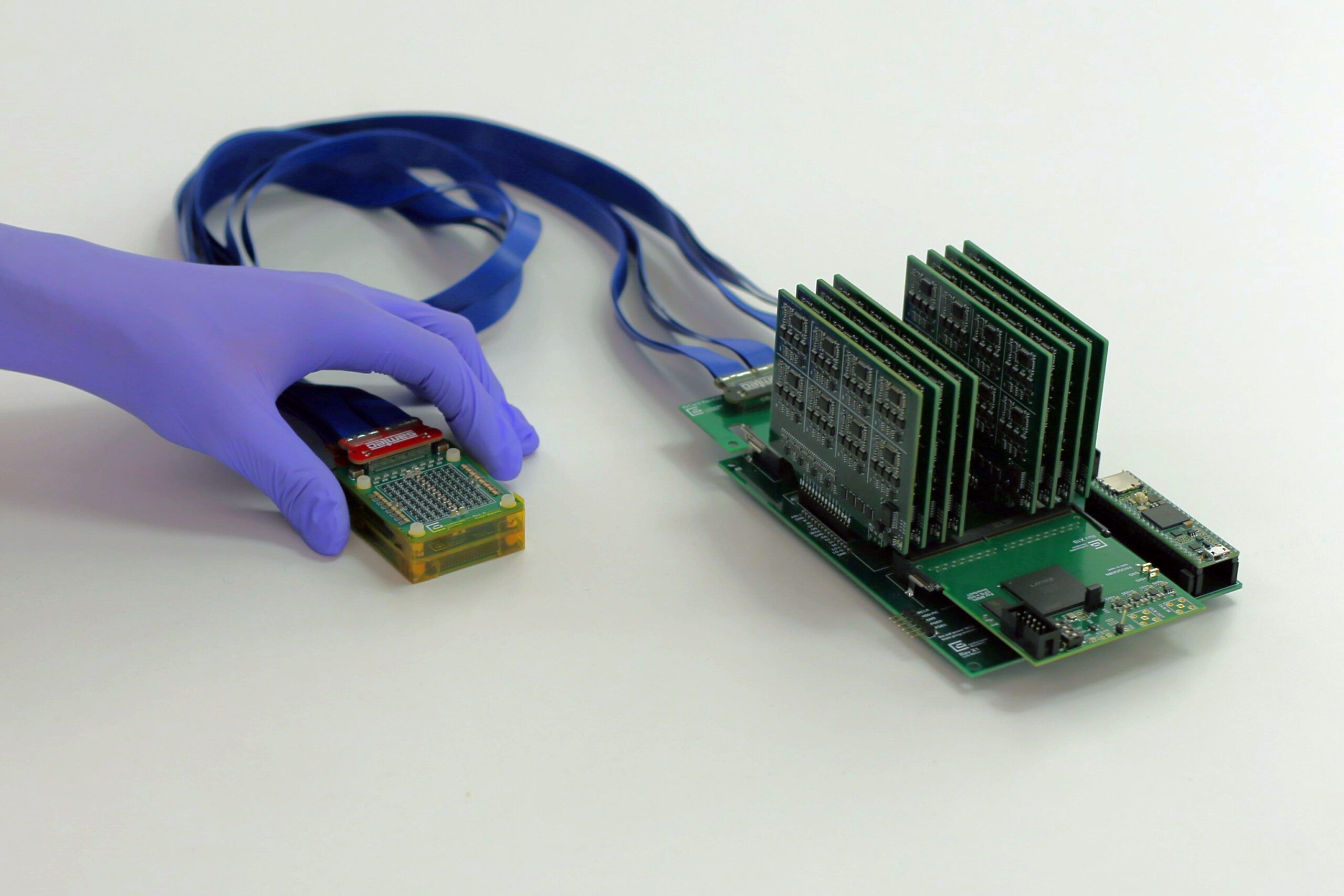
Papautsky contributed a microfluidic device, crafted from glass and plastic, measuring just a few inches long and containing channels slightly wider than a strand of hair. This device isolates cancer cells based on size, a process known as a liquid biopsy.
“CTCs are typically larger than white blood cells, which are larger than red blood cells. Cancer cells also tend to be softer and more moldable,” Papautsky noted. “When we put the blood into this device, we can filter out the CTCs without modifying or damaging the cells.”
In 2019, Papautsky’s team demonstrated that this method could identify cancer cells with 93% accuracy. The current study compares this method to a commercially available tool called EasySep, which uses magnetic separation. Papautsky highlighted that magnetic separation can be harsh, sometimes damaging the cells it aims to capture.
Advancements in Cancer Cell Isolation
The researchers tested both systems—EasySep and Papautsky’s method—using blood samples from pancreatic cancer patients. Remarkably, Papautsky’s method recovered eight times as many cancer cells and processed samples faster, in as little as 20 minutes.
“The method’s success is so important for asymptomatic cancers like pancreatic cancer, where a blood draw may be the only way to diagnose early,” Papautsky said.
Dr. Pier Giulianotti, a co-investigator and division chief of general, minimally invasive, and robotic surgery at the College of Medicine, emphasized the significance of these findings. “Science is based on little steps,” he remarked. “And this is a very good step. Most malignant cancers in humans spread through the bloodstream. Understanding how cancer cells are released into the bloodstream and being able to control this process is very, very important.”
The study’s collaborative team includes additional UIC researchers Celine Macaraniag, Ifra Khan, Alexandra Barabanova, Valentina Valle, and Alain Borgeat, with Jian Zhou of Rush University Medical Center as a coauthor.
This innovative research not only highlights the potential of lidocaine in reducing metastasis but also underscores the importance of interdisciplinary collaboration in advancing cancer treatment. As the study progresses, it may pave the way for more personalized and effective therapies for pancreatic cancer patients.