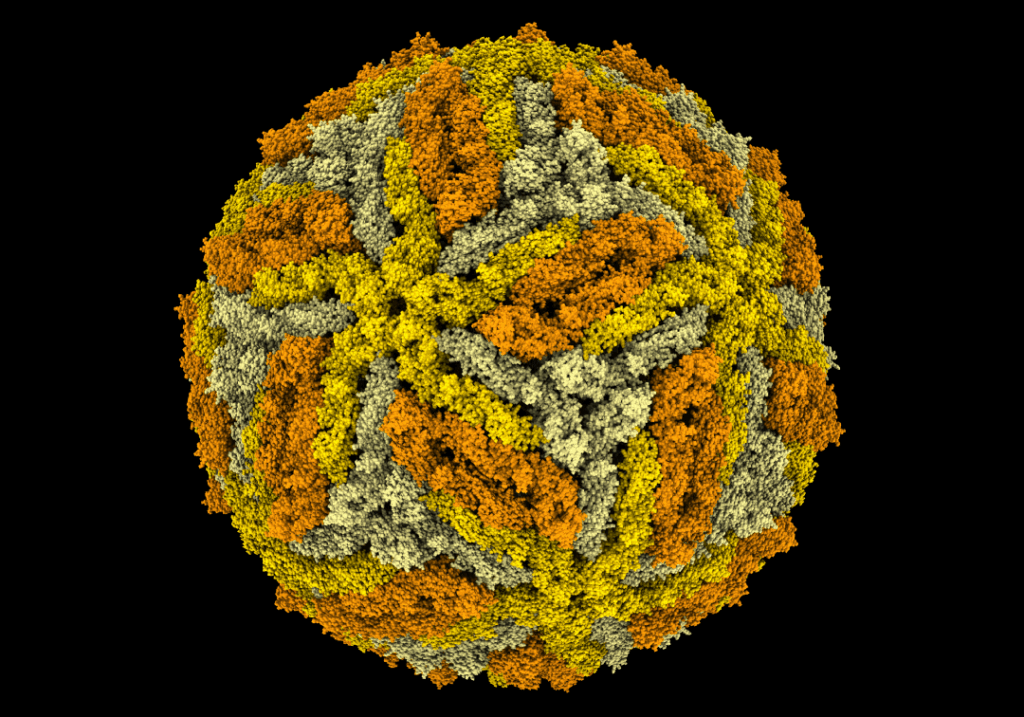
In a groundbreaking study, researchers at the University of Queensland (UQ) have unveiled structural differences between the vaccine strain of yellow fever (YFV-17D) and its virulent, disease-causing counterparts. This discovery marks the first time a complete 3D structure of a fully mature yellow fever virus particle has been recorded at near-atomic resolution, providing new insights into the virus’s biology.
Dr. Summa Bibby from UQ’s School of Chemistry and Molecular Bioscience highlighted the significance of this advancement. “By utilising the well-established Binjari virus platform developed here at UQ, we combined yellow fever’s structural genes with the backbone of the harmless Binjari virus and produced virus particles that could be safely examined with a cryo-electron microscope,” Dr. Bibby explained. The study revealed that the vaccine strain particles possess a smooth and stable surface layer, whereas the virulent strain particles exhibit bumpy, uneven surfaces.
Implications for Immune Response
The structural differences between the vaccine and virulent strains have profound implications for how the body’s immune system recognizes the virus. “The bumpier, irregular surface of the virulent strains exposes parts of the virus that are normally hidden, allowing certain antibodies to attach more easily,” Dr. Bibby noted. “The smooth vaccine particles keep those regions covered, making them harder for particular antibodies to reach.”
This finding is particularly crucial given that yellow fever remains a major public health concern in parts of South America and Africa. With no approved antiviral treatments, vaccination is the primary means of prevention. The discovery could pave the way for improved vaccine designs and antiviral strategies, not only for yellow fever but also for related viruses.
Broader Impacts on Vaccine Development
Professor Daniel Watterson, another key researcher in the study, emphasized the broader implications of these findings. “The yellow fever vaccine remains effective against modern strains and seeing the virus in such fine detail lets us better understand why the vaccine strain behaves the way it does,” he said. “We can now pinpoint the structural features that make the current vaccine safe and effective.”
These insights could also inform future vaccine designs for other orthoflaviviruses, such as dengue, Zika, and West Nile. The ability to visualize the virus at such a detailed level allows researchers to identify specific structural features that contribute to the efficacy and safety of vaccines.
Historical Context and Future Directions
Yellow fever has a long history as a significant public health threat, with outbreaks recorded as far back as the 17th century. The development of the YFV-17D vaccine in the 1930s was a major milestone in controlling the disease. However, the virus’s ability to mutate and adapt poses ongoing challenges for vaccine development and disease management.
The UQ study represents a significant step forward in understanding the virus at a molecular level, offering hope for more effective interventions. As Professor Watterson concluded, “The findings could even inform future vaccine design for related viruses like dengue, Zika, and West Nile.”
Looking ahead, researchers aim to leverage these insights to develop next-generation vaccines and antiviral treatments that can provide broader protection against a range of flaviviruses. This development follows a growing recognition of the need for innovative approaches to combat emerging infectious diseases.
As the global health community continues to grapple with the challenges posed by viral diseases, the work of UQ scientists underscores the importance of cutting-edge research in driving progress and safeguarding public health.






