The aging European population is poised to exacerbate the burden of antimicrobial resistance (AMR), a new study reveals. As the risk of serious bacterial infections increases with age, the continent may witness a surge in mortality and morbidity linked to AMR. This growing challenge underscores the urgency for targeted interventions and robust policy measures.
Researchers have highlighted the critical need to raise awareness among policymakers, drive investments into evidence-based interventions, and improve the understanding of factors influencing AMR rates. Modeling studies that incorporate demographic shifts are crucial for estimating future AMR burdens and assessing the impact of potential interventions.
Demographic Shifts and AMR
Previous work has shown that resistance prevalence in bloodstream infections (BSI) is significantly influenced by the age and sex of patients. For instance, methicillin-resistant Staphylococcus aureus (MRSA) prevalence increases with age and is more common in men. Similarly, aminopenicillin resistance in Escherichia coli declines with age but also shows a higher burden in men.
Across Europe, studies suggest that BSI rates are on the rise, particularly among older adults and men. However, comprehensive estimates of infection incidence rates by age and sex across Europe remain scarce. This gap in data complicates efforts to understand the full impact of demographic shifts on AMR.
Modeling Future Burdens
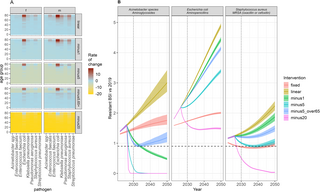
The study utilized a three-step modeling approach to estimate the future burden of BSIs with AMR in Europe through 2050. By calculating projected BSI incidence rates and combining these with demographic projections, researchers estimated age- and sex-specific BSI rates. A hierarchical modeling approach was then used to determine the number of antibiotic-resistant BSIs each year.
This approach revealed significant dynamics in three key bacteria-antibiotic combinations: E. coli-aminopenicillin resistant, S. aureus-methicillin resistant, and Acinetobacter spp-aminoglycoside resistant. Notably, the study found substantial variation in AMR burden projections across different European countries.
Implications for Policy and Interventions
The study’s findings align with prior research indicating increased BSI incidence among older adults and men. While EARS-Net was not explicitly designed to monitor infection incidence trends, the importance of supplementing AMR data with infection incidence estimates is increasingly recognized.
Researchers emphasize the need for stratified analyses to refine AMR burden estimates and intervention strategies. The study highlights that failure to account for age and sex in resistance burden estimations may lead to significant over- or under-estimation of resistant cases, particularly in older populations.
“Even with very successful public health interventions, 32% of the included bacteria-antibiotic combinations would not achieve a 10% reduction in infection burden by 2030,” the study notes.
Challenges and Future Directions
Long-term projections of AMR are inherently challenging, with dynamic factors influencing resistance burdens. The study refrains from labeling its projections as forecasts, instead presenting them as conditional projections based on current trends.
Driven by high-quality data, the study’s methodology could be applied to other settings with representative data. However, the lack of comprehensive data on age- and sex-stratified case fatality rates (CFRs) complicates efforts to focus on incidence reduction.
Future research is needed to explore country-level variations in resistance burdens and to understand how incidence burdens translate to variable mortality burdens. The study underscores the importance of incorporating demographic shifts into AMR burden projections and emphasizes the need for tailored intervention strategies.
Conclusion
The study represents a significant advance in incorporating demographic shifts into AMR burden projections in Europe. It highlights the importance of age and sex disaggregation in burden assessments and the challenges in achieving AMR targets amid demographic changes.
As Europe faces an aging population, immediate action is required to mitigate the anticipated rise in resistance burdens. Sustained efforts in surveillance, tailored interventions, and demographic-specific policy measures are crucial to effectively combating AMR and reducing the future burden of bloodstream infections.
The findings underscore the necessity of stratified analyses by different bacteria-antibiotic combinations, supported by improved data disaggregation. While projections to 2050 remain uncertain, the study calls for immediate and sustained action to address the growing AMR challenge.






