In a groundbreaking effort to combat one of the deadliest forms of cancer, a new phase II study is investigating the efficacy of stereotactic body radiation therapy (SBRT) in treating inoperable, non-metastasized pancreatic ductal adenocarcinoma (PDAC). This study, known as TORPEDO, aims to improve progression-free survival (PFS) by integrating SBRT with systemic chemotherapy.
Pancreatic ductal adenocarcinoma is notorious for its aggressive nature and late-stage diagnosis, making it the third leading cause of cancer-related deaths globally. According to the Belgian Cancer Registry, the incidence of pancreatic cancer is rising, with an annual increase of 2.7% in males and 3.4% in females. Radical surgical resection remains the only potential cure, but only 15% of patients are eligible due to the late onset of symptoms.
The Challenge of Locally Advanced Pancreatic Cancer
Locally advanced pancreatic cancer (LAPC) presents a significant challenge, with 35% of patients diagnosed at this stage. Historically, chemotherapy regimens like 5-fluorouracil and gemcitabine have been used, but the introduction of FOLFIRINOX in 2011 marked a turning point, offering superior overall survival rates.
Despite advances, local disease progression remains a critical issue. Autopsy studies reveal locoregional failure rates between 28% and 63%, with local disease directly causing death in up to 30% of cases. The integration of radiation therapy, particularly SBRT, into treatment regimens is seen as a promising approach to reduce local recurrence and enhance the potential for curative surgery.
SBRT: A Precision Approach
Stereotactic body radiation therapy is a precise technique delivering high doses of radiation to a targeted area, minimizing exposure to surrounding organs. This method is already a standard for early-stage lung and prostate cancers and is now being explored for pancreatic cancer.
Early studies, such as those by the Stanford group, demonstrated the potential of SBRT in LAPC, showing promising results in local control (LC) and overall survival (OS). More recent studies have reported improved outcomes when SBRT is combined with chemotherapy, compared to chemotherapy or chemoradiotherapy alone.
In a matched case-control study, SBRT showed a 1-year LC rate of 80% versus 53% with chemoradiotherapy, and a 2-year LC of 50% versus 40% (p = 0.017).
The TORPEDO Study: A New Hope
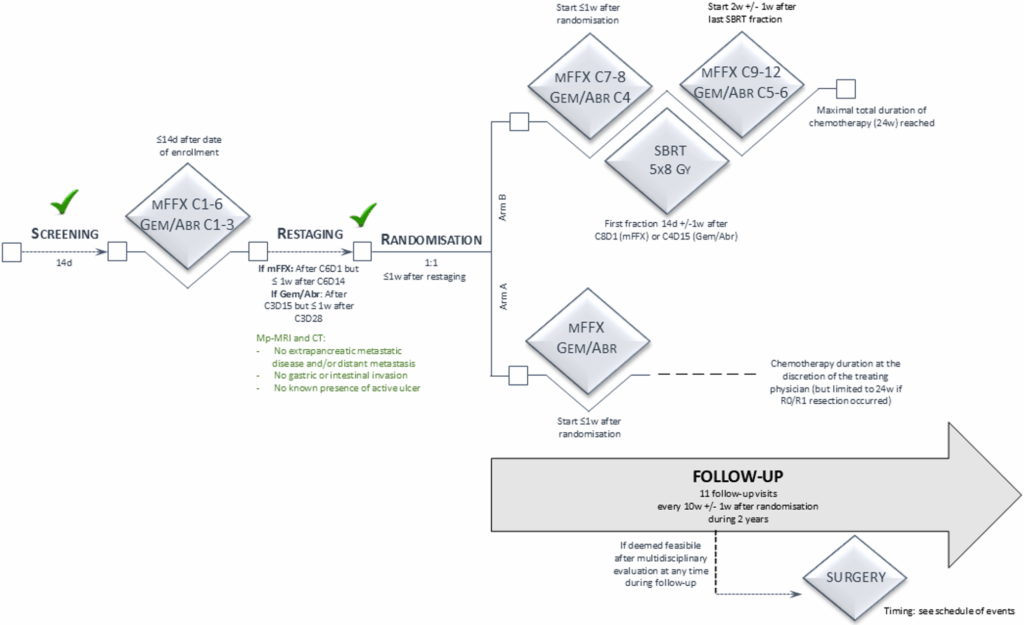
The TORPEDO study aims to evaluate the effectiveness of adding SBRT following induction chemotherapy in patients with inoperable, non-metastasized PDAC. Conducted across fourteen centers in Belgium and one in the Netherlands, the study includes patients with LAPC and borderline resectable pancreatic cancer (BRPC) who are inoperable due to medical conditions or personal choice.
Participants receive twelve weeks of induction chemotherapy, followed by randomization to either continue chemotherapy or receive SBRT. The primary objective is to compare the 2-year PFS between the two groups, with secondary endpoints including overall survival, metastasis-free survival, and quality of life.
“The integration of SBRT with systemic treatment may lead to improved progression-free survival compared to chemotherapy alone,” the study hypothesizes.
Implications and Future Directions
The TORPEDO study represents a significant step forward in the treatment of pancreatic cancer, offering hope for improved outcomes in a disease historically marked by poor prognosis. By focusing on local control and integrating advanced radiation techniques, the study seeks to enhance the quality of life and survival rates for patients with inoperable PDAC.
As the study progresses, its findings could pave the way for new standards in treating pancreatic cancer, potentially transforming the therapeutic landscape and offering new hope to patients worldwide.
The results of this study could have far-reaching implications, not only improving survival rates but also setting a precedent for the integration of advanced radiation techniques in other challenging cancer types.






