In a remarkable turnaround, Australia has reported a significant decrease in mpox cases in 2025 compared to the previous year. During a three-month period in 2024, the country saw a surge in infections, with over 600 of the year’s total 1,409 cases recorded between July and September. However, as of October 22, 2025, only 203 cases have been confirmed nationwide, with the majority occurring in Victoria and New South Wales, according to the Department of Health.
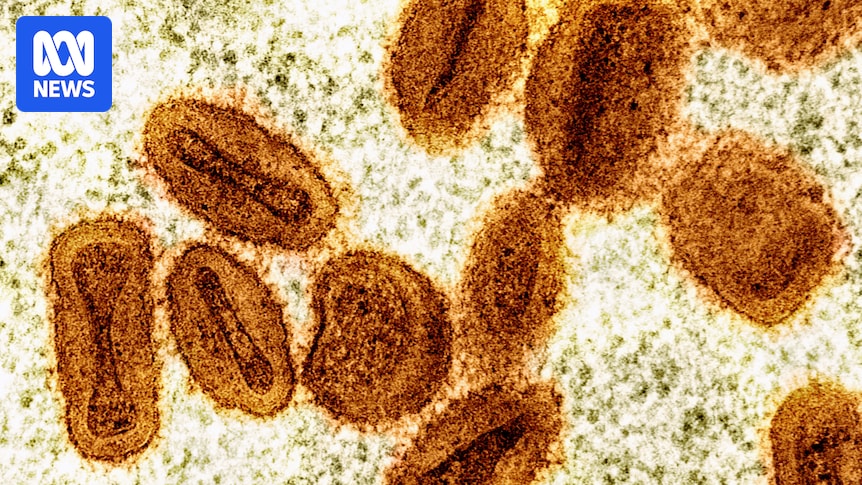
Mpox, a virus related to smallpox, spreads through intimate or physical contact and can be transmitted via skin, body fluids, or contaminated materials. Though endemic to parts of West and Central Africa, recent years have seen disproportionate impacts on gay and bisexual men, as well as other men who have sex with men (GBMSM), in Australia, Europe, and North America.
Understanding the 2024 Surge
The spike in mpox cases last year can be attributed to several factors. Andrew Grulich, an epidemiologist and scientia professor at the University of New South Wales’s Kirby Institute, explains that Australia’s delayed access to vaccines played a significant role. “Australia is different to many other high-risk countries because we didn’t get the vaccine until relatively late in that first year, about September 2022, while many countries in northern Europe and North America had access in June and July,” he noted.
Professor Grulich highlighted the fear associated with the virus’s rapid spread, which led to severe cases, particularly among people living with HIV. “Even when it wasn’t severe, it was often quite noticeable with lesions on the arms, legs, and genitals,” he added.
“There were 115,265 vaccine doses administered from 2022 to 2024. As of earlier this month, 19,435 have received one or more doses since January this year.”
According to a GBQ+ survey by UNSW’s Centre for Social Research in Health, vaccination uptake has increased slightly in 2025, with 48.8% of respondents completing the two-dose schedule, compared to 39.9% in 2024.
Factors Behind the 2025 Decline
Arthur Wong, a sexual health specialist and conjoint lecturer at Kirby Institute, attributes this year’s lower case numbers to a robust public health response. “We raised quite high levels of public awareness of symptoms, which helps reduce onward transmission, but also we managed to increase vaccination in high-risk groups,” Dr. Wong explained.
Vaccination efforts were focused on gay and bisexual men, GBMSM with multiple partners, trans and gender-diverse people, and those engaged in sex work. “Mpox is an infection that gives some quite-lasting immunity protection after natural infection and vaccination,” he noted, emphasizing the importance of completing the two-dose vaccine schedule.
Melbourne-based sexual health clinician Jason Ong pointed out that changes in sexual behavior also contributed to the decline. “At the height of the mpox epidemic, a lot of GBMSM had safer sex or reduced partners, and that had a massive impact on cases,” he said.
Potential Underreporting and Future Concerns
Despite the positive trend, Professor Ong cautioned about potential underreporting of mpox symptoms. “Mpox doesn’t always cause severe disease, so it can be mild, or people might not have symptoms at all,” he explained. This could mean that actual case numbers are higher than reported, as individuals may not seek medical attention.
“Only if we get vaccination rates up further can we be quite certain we won’t see a large outbreak,” Professor Grulich emphasized.
The Jynneos vaccine, which requires two doses, is now widely available, but small cluster outbreaks remain a possibility. Professor Grulich stressed the need for continued focus on a vaccination-based approach to prevent large outbreaks.
Monitoring Variants and Future Preparedness
The mpox virus is divided into two clades, with clade 2 being the predominant variant in Australia. However, clade 1, associated with more severe illness, is being closely monitored by public health officials. “The variant we currently have circulating in Australia is clade 2, but there is a more serious version, which is in Central Africa,” Professor Ong said.
So far, only two cases of the more severe clade 1b have been detected in Australia, both linked to overseas travel. This highlights the importance of vigilance and preparedness in managing potential future outbreaks.
As Australia continues its efforts to control mpox, the focus remains on increasing vaccination rates and monitoring viral variants to ensure public health safety.