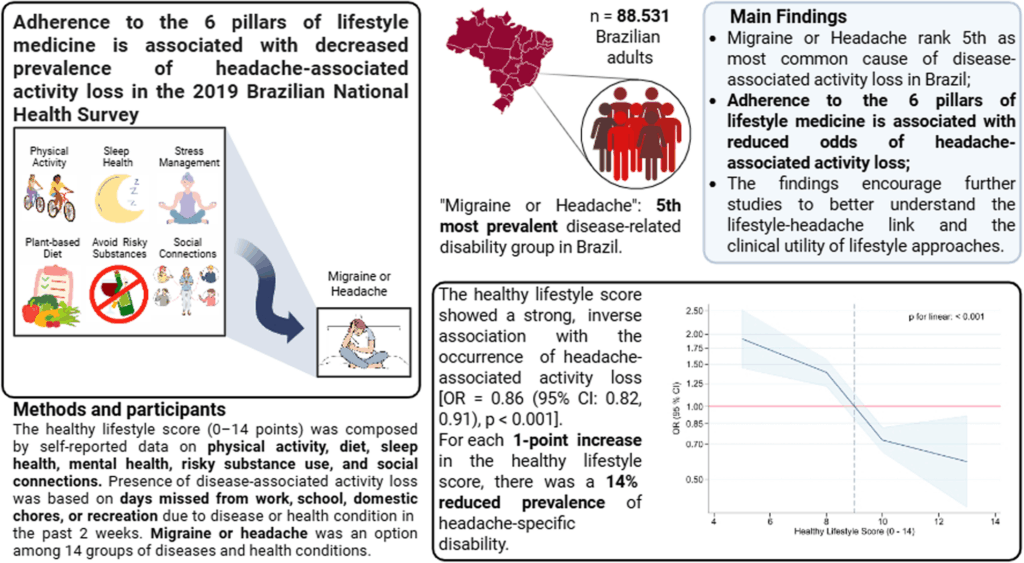
A recent study has highlighted the potential of lifestyle medicine in mitigating headache-related disabilities in Brazil. This research, a subanalysis of the PNS2019 database, examined the correlation between lifestyle factors and headache-associated activity loss across the Brazilian population. Conducted by the Ministry of Health in collaboration with the Fundação Oswaldo Cruz (Fiocruz) and Instituto Brasileiro de Geografia e Estatística (IBGE), the study spanned from August 2019 to March 2020.
The PNS2019 survey employed a complex sampling design to gather data from 90,846 participants, achieving a 96.5% response rate. The focus was on Brazilian adults aged 18 and above, who provided information on sociodemographic factors, health service utilization, lifestyle behaviors, and chronic diseases. The study received approval from the National Research Ethics Committee, ensuring ethical compliance throughout.
Understanding Headache-Associated Activity Loss
Headache-associated activity loss was assessed by questioning participants about the number of days they were unable to perform daily activities due to health conditions. “Headache or Migraine” was among the 14 health conditions listed. The study found that headache-related activity loss was the fifth most common cause of disease-associated activity loss in Brazil, affecting approximately 751,092 Brazilian adults.
Participants lost an average of 3.5 days over two weeks due to headaches, with the condition being particularly prevalent among women and young adults aged 18 to 35. The study revealed significant sociodemographic disparities, with higher prevalence among females, individuals from the Northeast region, and those with lower education and income levels.
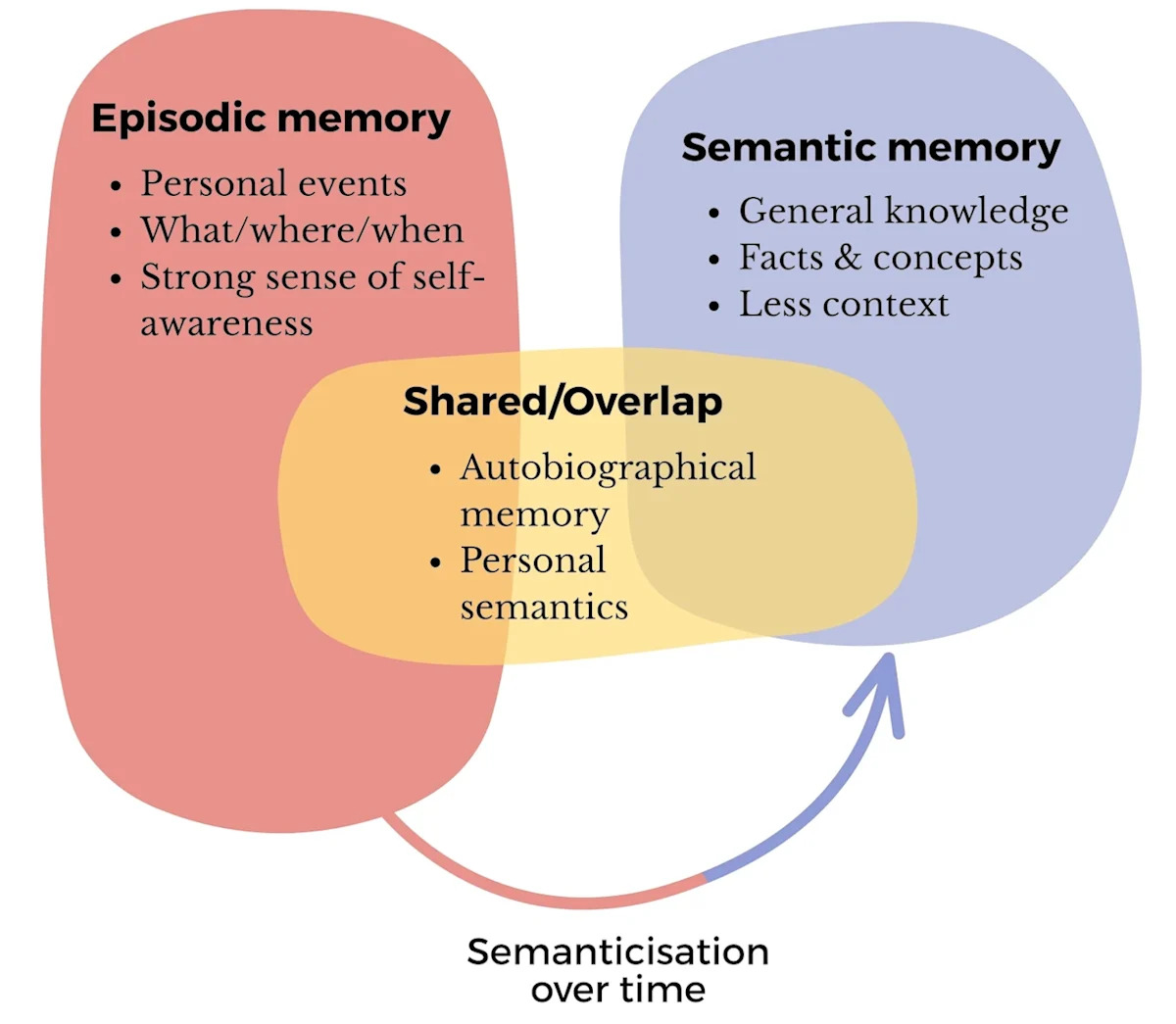
The Six Pillars of Lifestyle Medicine
The study utilized a “healthy lifestyle score” based on the six pillars of lifestyle medicine: physical activity, sleep health, diet, mental health, risky substances, and social connection. Each component was scored from 0 to 2, with higher scores indicating healthier lifestyle choices. The total score ranged from 0 to 14, with higher scores reflecting a healthier lifestyle profile.
Physical Activity and Diet
Physical activity was a key factor, with participants categorized as “active,” “somewhat active,” or “inactive” based on their adherence to WHO guidelines. Dietary patterns were assessed using a Food Frequency Questionnaire, with scores assigned based on the consumption of healthy and unhealthy food groups.
Sleep and Mental Health
Sleep health was evaluated through questions about sleep medication use and sleep problems, while mental health was assessed using the PHQ-9 scale for depression severity. Both factors showed strong inverse associations with headache-related activity loss.
Risky Substances and Social Connections
Smoking and alcohol consumption were analyzed under the “risky substances” pillar, with non-smokers and abstemious individuals scoring higher. Social connections were assessed through participation in group activities, with regular engagement linked to better health outcomes.
Statistical Analysis and Findings
The study employed binary logistic regression models to explore the associations between lifestyle scores and headache-associated activity loss. The findings indicated a strong inverse relationship, with each one-point increase in the healthy lifestyle score reducing the odds of headache-associated activity loss by 14%.
The adjusted models showed that higher adherence to physical activity, sleep health, and mental health significantly reduced the odds of headache-associated activity loss.
Interestingly, a “U” shaped relationship was observed with diet, where moderate adherence was most beneficial. Conversely, high adherence to drinking and smoking showed increased odds of headache-associated activity loss, suggesting complex interactions between these factors.
Implications and Future Directions
The study underscores the potential of lifestyle modifications in reducing headache-related disabilities, complementing pharmacological therapies. The findings align with global research, highlighting the need for public health strategies that incorporate lifestyle interventions.
Experts suggest that addressing modifiable behaviors could enhance recovery and quality of life for individuals with headaches. The study advocates for the inclusion of headache-specific strategies in national health programs, emphasizing the role of lifestyle medicine in public health.
While the study provides valuable insights, its cross-sectional design limits causal inferences. Future research should explore longitudinal relationships between lifestyle factors and headache prevalence, considering the complex interplay of individual components.
Overall, the findings highlight the importance of a holistic approach to headache management, integrating lifestyle medicine with traditional treatments to improve patient outcomes and reduce the burden of headache disorders in Brazil.