Researchers at the University of Arizona have identified a potential link between chronic pain and a rare immune condition, potentially paving the way for future research into immune biomarkers for chronic pain. This discovery emerged from a study led by Dr. Julie Pilitsis, a professor and chair of the Department of Neurosurgery at the University of Arizona College of Medicine – Tucson.
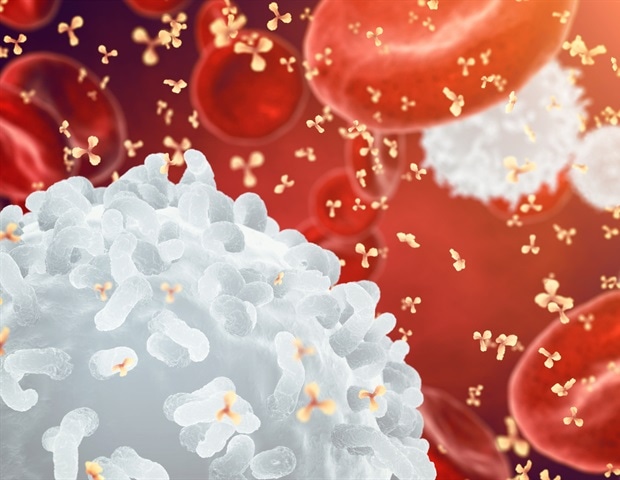
The study, which analyzed medical records, found that 12% of chronic pain patients treated with spinal cord stimulation or an implanted pain medicine pump exhibited a white blood cell condition known as eosinophilia. Typically, eosinophilia is seen in less than 1% of the general population, indicating a significant deviation among chronic pain sufferers.
Understanding Eosinophilia and Its Implications
Eosinophilia is characterized by an elevated number of eosinophils, a type of white blood cell involved in defending against allergens and protecting the body from fungal and parasitic infections. The condition is often linked to autoimmune and chronic inflammatory diseases. Dr. Pilitsis, who is also a member of the University of Arizona Comprehensive Center for Pain and Addiction, noted that chronic pain is increasingly believed to involve an inflammatory component.
“Few studies have examined a connection between eosinophilia and pain,” Pilitsis stated. “We’re always looking for risk factors to identify and modify – and which ideally could help us predict who will respond to chronic pain treatment.”
The findings were published in the journal Neuromodulation: Technology at the Neural Interface, highlighting the potential for eosinophilia to serve as a biomarker in chronic pain management.
Exploring the Connection Between Pain and the Immune System
According to the U.S. Centers for Disease Control and Prevention, approximately 24.3% of U.S. adults experience chronic pain, with 8.5% suffering from high-impact chronic pain that significantly affects daily life. Patients receiving spinal cord stimulation or a pain medicine pump often belong to this latter group.
Spinal cord stimulators are devices implanted to send low levels of electricity into the spinal cord to alleviate pain, while intrathecal pain pumps deliver medication directly into the fluid surrounding the spinal cord. Dr. Pilitsis and her team reviewed the medical records of 212 patients who underwent these treatments for high-impact chronic pain, focusing on 114 patients who had routine blood tests before treatment.
“The condition typically affects fewer than 1 in 100 people, and we found 14 of 114, or roughly 12%, in this group had eosinophilia before treatment,” Pilitsis explained. “Now we’re asking what is it about eosinophilia that might predispose someone to chronic pain?”
Potential for Future Research and Treatment Approaches
While approximately 70% of spinal cord stimulation patients experience some pain reduction, the role of eosinophilia in treatment outcomes remains unclear. Dr. Pilitsis speculated on the potential for spinal cord stimulation to reduce inflammation and whether eosinophilia could serve as a marker for treatment efficacy.
“It’s just speculation, but for those who don’t do well, we could think of adding an anti-inflammatory to the chronic pain treatment. We still have many questions,” she noted.
Interestingly, inflammatory conditions like rheumatoid arthritis did not correlate with eosinophilia, suggesting that the relationship between chronic pain and the immune system is complex and warrants further investigation.
Collaborative Efforts and Future Directions
The research team included Dr. Martin Weinand, professor of neurosurgery, and medical students Hanna Johnson and Avantika Mitbander from the University of Arizona. Additional contributions came from Emma Sargent of Florida Atlantic University and Dr. Henry Skelton, a pre-residency fellow at the College of Medicine – Tucson.
This study opens the door to exploring new avenues in chronic pain management, particularly in identifying biomarkers that could predict patient responses to treatment. As research continues, the hope is to develop more personalized and effective strategies for those suffering from chronic pain.