The global population is rapidly aging, with the proportion of individuals aged 60 and above projected to rise from 12% in 2020 to 22% by 2050. In Malaysia, the elderly population is expected to reach 15% by 2030. As this demographic shift occurs, healthcare providers face the dual challenge of managing both physical and mental health issues in older adults.
While chronic diseases and cognitive decline are well-documented concerns, mental health issues such as depression and anxiety are increasingly recognized as significant public health challenges among the elderly. According to the World Health Organization, 7% of the global elderly population experiences depression, with 3.8% suffering from anxiety, contributing to 6.6% of all disabilities measured in disability-adjusted life years (DALYs).
The Role of Nutrition in Mental Health
Emerging research highlights the crucial role of nutritional status in influencing mental health outcomes among older adults. Malnutrition, defined by the European Society of Clinical Nutrition and Metabolism (ESPEN) as a state resulting from inadequate nutrition intake or uptake, has been linked to diminished physical and mental function. It is associated with increased psychological distress, depression, and anxiety.
Recent studies suggest that the gut-brain axis, a communication system between the gut and brain, may mediate the effects of nutrition on mental health, although the mechanisms remain under investigation. Despite these associations, nutritional status is often overlooked in older adults’ care as a contributing factor to mental health problems.
Study Design and Methodology
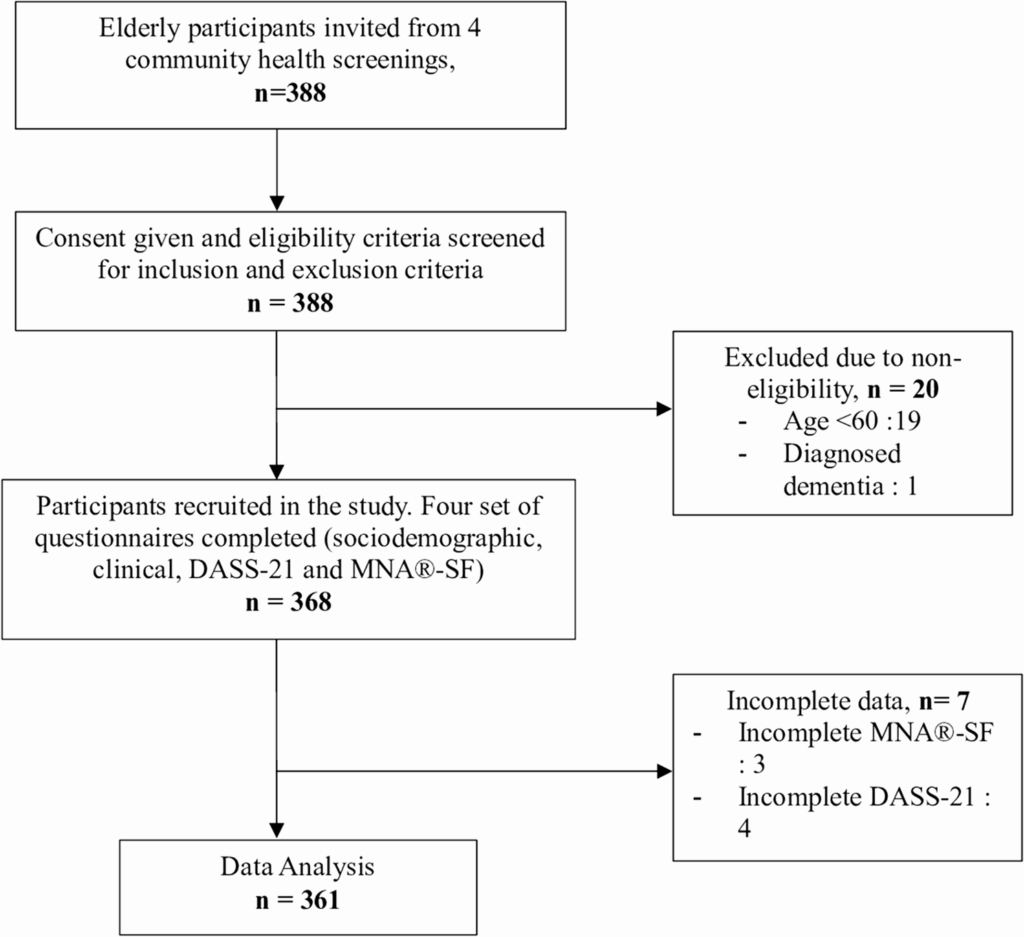
A recent cross-sectional study conducted in Kuala Selangor District, Malaysia, sought to investigate the association between nutritional status and mental health outcomes among elderly individuals. The study involved 361 participants aged 60 and above, attending community health screenings from June to October 2024. The study utilized the Depression, Anxiety, and Stress Scale-21 (DASS-21) and the Mini Nutritional Assessment-Short Form (MNA®-SF) to assess mental health and nutritional status, respectively.
The findings revealed that 23% of participants were at risk of malnutrition, while 6.4% were classified as malnourished. Mental health assessments indicated that 12.7% experienced depression, 9.4% had anxiety, and 4.2% suffered from stress. The study identified significant associations between nutritional status and mental health, with malnutrition linked to higher odds of depression and anxiety.
Implications and Expert Opinions
The study’s findings underscore the importance of integrating nutritional assessments into geriatric care. Dr. Aisha Rahman, a geriatric specialist, emphasized the need for a multidisciplinary approach, stating,
“Addressing nutritional deficiencies in older adults can significantly improve their mental health outcomes. It’s crucial for healthcare providers to consider nutrition as a key factor in managing depression and anxiety in this population.”
Internationally, similar studies have reported elevated depression rates among malnourished elderly individuals, highlighting the global relevance of these findings. However, the study’s authors caution that the strong associations observed should be interpreted with care due to the small sample size and potential for residual confounding.
Future Directions and Recommendations
To enhance the well-being of the elderly population, the study recommends implementing community-based meal programs, home-delivered nutrition support, and nutrition education workshops tailored for older adults. Social support programs, such as senior activity centers and peer support groups, can also help reduce isolation and improve mental health.
For future research, longitudinal studies are needed to explore the causal relationship between malnutrition and mental health disorders in elderly individuals. Investigating sociodemographic and lifestyle factors can help refine targeted interventions and improve early detection strategies. Additionally, research on the effectiveness of dietary modifications and personalized interventions can help mitigate nutritional risk and mental health decline.
Conclusion
This study highlights the critical link between nutritional status and mental health among the elderly, emphasizing the need for comprehensive care that addresses both physical and mental health needs. As the global population continues to age, integrating nutritional assessments into geriatric care will be essential in improving the quality of life for older adults.