Patients with recurring prostate cancer are experiencing a significant breakthrough in treatment, thanks to a new PSMA-targeted radioligand therapy. Recent clinical trial results from UCLA Health Jonsson Comprehensive Cancer Center reveal that this therapy, when administered before stereotactic body radiotherapy (SBRT), more than doubles the time patients go without disease progression compared to SBRT alone. These findings were presented at the 2025 American Society for Radiation Oncology Annual Meeting in San Francisco.
The study demonstrated that men receiving the radioligand drug experienced a median progression-free survival of 17.6 months, compared to just 7.4 months for those treated with SBRT alone. This delay translates into a significant postponement in the initiation of hormone therapy, a common treatment for recurrent prostate cancer that often comes with severe side effects such as fatigue and bone loss.
Breakthrough in Prostate Cancer Treatment
“This is the first randomized trial to show that PSMA-targeting radioligand can significantly delay progression when added to metastasis-directed radiation,” stated Dr. Amar Kishan, executive vice chair of radiation oncology at the David Geffen School of Medicine at UCLA and the study’s first author. “It gives patients more time before needing hormonal therapy, which can carry significant side effects. Avoiding or delaying hormonal therapy consistently benefits quality of life.”
Prostate cancer ranks as the second most common cancer among men globally. For many, the disease returns years after initial treatment, manifesting as a few new lesions—a stage known as oligorecurrent disease. SBRT has become a prevalent method for treating these cases, focusing on visible lesions while sparing healthy tissue. However, the challenge of microscopic disease, undetectable by imaging scans, often leads to relapse.
Innovative Use of Radioligand Therapy
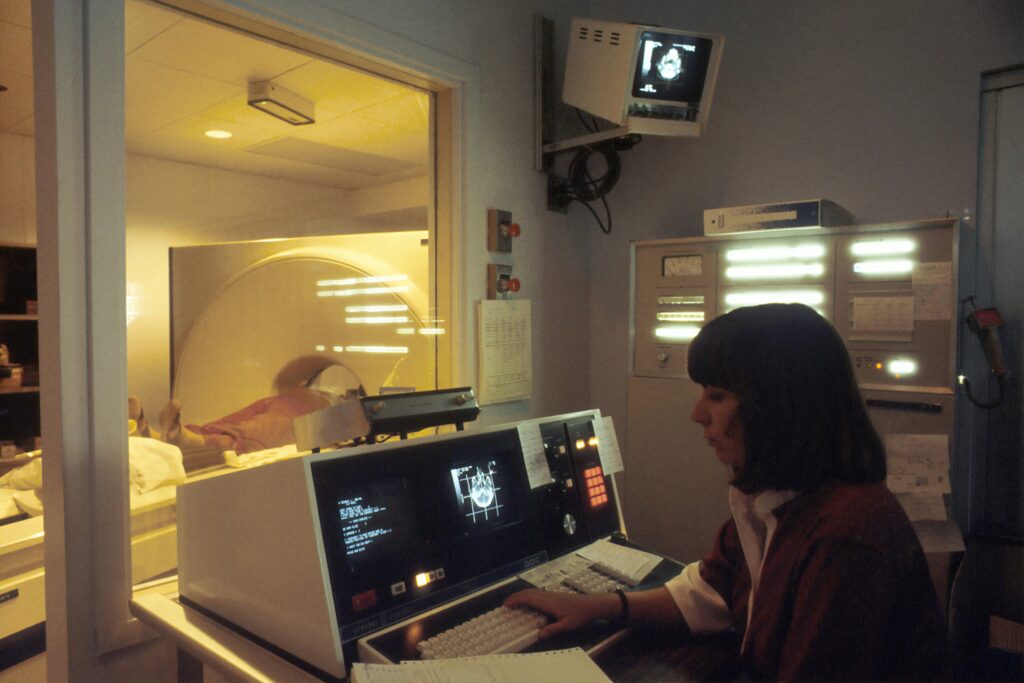
The phase 2 LUNAR trial investigated the potential of adding a radioactive drug, PNT2002, which targets PSMA—a protein highly expressed on prostate cancer cells—before SBRT to manage these hidden tumors. Dr. Jeremie Calais, senior author and director of the Ahmanson Translational Theranostics Division’s clinical research program, emphasized the trial’s significance: “We leveraged PSMA PET imaging technology to guide SBRT targeting, which is more precise than other imaging methods. And we combined it with PSMA radioligand therapy to treat PSMA expressing sites of disease, both visible and microscopic.”
The study involved 92 men with recurrent prostate cancer, randomly assigned to receive either SBRT alone or two doses of 177Lu-PNT2002 followed by SBRT. The researchers monitored patients using regular PSA blood tests and PSMA PET scans to determine the duration of cancer-free progression.
Adding 177Lu-PSMA before SBRT more than doubled progression-free survival, extending it from 7.4 months to 17.6 months, reducing the risk of cancer returning, the need for hormone therapy, or death by 63%.
Implications and Future Directions
Despite the clear benefits, 64% of men still experienced disease progression, highlighting the ongoing challenge of microscopic cancer. Dr. Kishan noted, “This is an important proof of principle. It suggests we may be able to intervene earlier with radioligand therapy and meaningfully change the course of disease. Importantly, we didn’t see significantly worse side effects with the addition of the drug.”
The research team also identified biological markers that may predict which patients will benefit most from the treatment. A stronger immune response post-SBRT, indicated by T cell receptor changes, correlated with better outcomes. Additionally, a set of 20 genes linked to immune function and DNA repair helped define patients at varying risk levels for progression.
Dr. Calais added, “This work exemplifies true collaboration between radiation oncology and nuclear medicine, showcasing theranostics at its best—a mix of imaging and therapy.”
Further research is necessary to track long-term outcomes and explore other methods to optimize response rates. The study, funded by Lantheus, involved numerous UCLA authors, including Luca F. Valle, Holly Wilhalme, Carol Felix, and many others, contributing to the comprehensive analysis and understanding of this innovative treatment approach.