Efforts to reduce unnecessary antibiotic use are yielding positive results, according to researchers from The University of Western Australia (UWA). Their study reveals a significant decline in the number of antibiotics dispensed to Australian children over the past decade, marking a crucial step in combating antimicrobial resistance (AMR).
Overuse or misuse of antibiotics is a primary driver of AMR, a global health threat recognized by the World Health Organization (WHO) and governments worldwide. AMR renders once-reliable antibiotics ineffective, contributing to an estimated 1.14 million deaths globally in 2021. Projections suggest it could claim 39 million lives and cost the global economy up to $10 trillion by 2050.
Research Findings Highlighting a Decade of Progress
New research from UWA’s School of Population and Global Health, led by Dr. Erin Kelty, indicates that Australian doctors are making strides in reducing the incorrect or over-prescription of antibiotics. The study, published in Paediatric and Perinatal Epidemiology, shows a marked decrease in antibiotics dispensed to children from 2013 to 2023.
Using data from the Pharmaceutical Benefits Scheme (PBS), researchers examined trends in antibiotic dispensing to children under 13. The team analyzed over 3.4 million prescriptions dispensed to 554,837 children, representing 10% of the PBS’s full dataset.
In 2013, there were 103 prescriptions dispensed for every 100 children. By 2023, this number had fallen to 63 per 100 children.
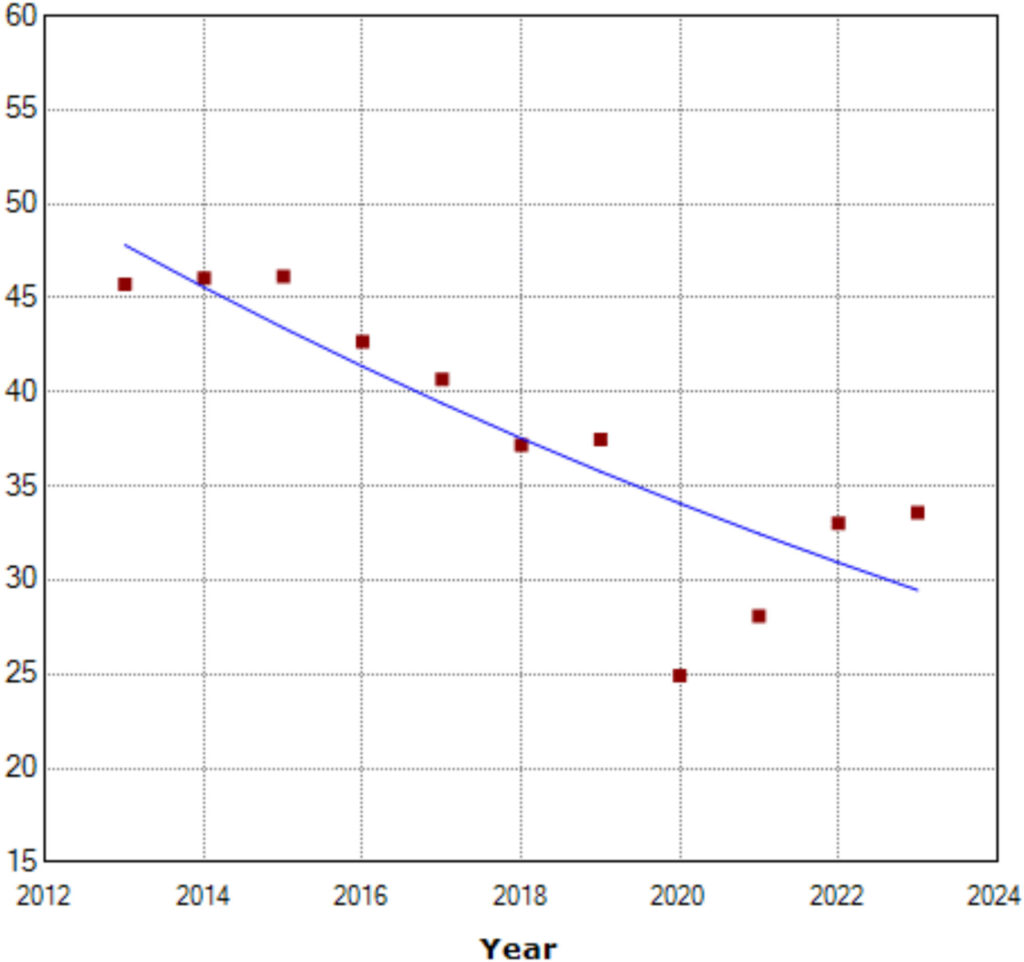
“The proportion of children dispensed with an antibiotic each year also decreased, with 45.7% of children receiving an antibiotic in 2013 compared to 33.6% in 2023,” Dr. Kelty noted.
Impact on Antibiotic Types and Economic Savings
The reduction in prescriptions was observed across sex, age, and most antibiotic types, with the most significant drop in “Watch” antibiotics. These broad-spectrum antibiotics are typically more costly and reserved for severe conditions or resistant bacterial infections.
“Dispensing of ‘Watch’ antibiotics dropped substantially, decreasing by 15% each year,” Dr. Kelty said. “In 2013, these antibiotics represented 17% of all antibiotics dispensed to children; by 2023, this had dropped to 6.4%.”
This decline translated into substantial financial savings for consumers and the PBS. The average prescription cost per 100 children decreased from $471 per year in 2013 to $274 in 2023, resulting in a total saving of $669,509 annually over the decade.
“Given our results are based on a 10% sample of PBS data, this reflects an estimated saving of approximately $6.7 million annually in dispensing of government-subsidized medicines in Australia from antibiotics alone,” Dr. Kelty explained.
Challenges and Future Directions
Despite these promising results, Australia still ranks high in antibiotic use compared to other high-income countries like the United Kingdom, Germany, Switzerland, and Norway. Dr. Kelty emphasized that children receive more antibiotics than most other age groups due to their developing immune systems and parental pressure on doctors to prescribe antibiotics.
“Our findings suggest that efforts to educate parents, consumers, and doctors about the importance of using antibiotics only when necessary are aligning with national public health goals to combat AMR,” Dr. Kelty said. “The reduction also means fewer children are exposed to the risk of negative side effects associated with antibiotics.”
Co-author Ebony Quintrell, a Ph.D. candidate with UWA and The Kids Research Institute Australia, highlighted the need for ongoing efforts. “Continuous monitoring of broad-spectrum antibiotics and dispensing trends will be crucial to sustain efforts to combat AMR,” Quintrell stated. “We also need to improve testing and identification of bacteria to prescribe antibiotics more effectively.”
As Australia continues to address the challenges of AMR, the study underscores the importance of informed antibiotic use and the ongoing need for vigilance in prescription practices. The progress made over the past decade offers a hopeful outlook for future public health initiatives aimed at reducing AMR’s impact globally.







